At Living Free, we often meet people who have been through years of psychiatric treatment, multiple diagnoses, and countless medications, yet still feel something is deeply wrong. One of the most common stories we hear is this: “My doctor says I’m bipolar, but the medication isn’t working.”
According to Dr. Reshie Joseph, Clinical Director and Psychotherapist at Living Free, misdiagnosing trauma as bipolar disorder is one of the biggest problems in mental health today.
“Bipolar disorder is classified as a disorder of mood. Trauma is a disorder of stress. On the surface, they can look the same, but the underlying cause is very different.” – Dr. Reshie Joseph
What Is Bipolar Disorder?
Bipolar disorder (formerly called manic-depressive illness or manic depression) is a mental illness that causes clear shifts in a person’s mood, energy, activity levels, and concentration.
According to the National Institute of Mental Health (NIMH):
“People with bipolar disorder often experience periods of extremely ‘up,’ elated, irritable, or energized behavior (known as manic episodes) and very ‘down,’ sad, indifferent, or hopeless periods (known as depressive episodes).” – NIMH
These mood episodes can last days, weeks, or even months. The “up” period may include racing thoughts, little need for sleep, risky behavior, or bursts of creativity, while the “down” period may involve overwhelming sadness, low energy, difficulty concentrating, or suicidal thoughts.
Causes and Symptoms of Bipolar Disorder
The exact cause of bipolar disorder isn’t fully understood. Still, suggests it may result from a combination of genetic, brain structure, and function differences, and environmental factors such as stress or trauma.
Bipolar Disorder Symptoms
- Intense mood swings between mania and depression
- Periods of excessive energy, reduced need for sleep
- Racing thoughts and rapid speech
- Risky or impulsive behaviors during manic phases
- Prolonged sadness or hopelessness
Read More: Avoidance in PTSD: A Hidden Cycle of Coping and Harm
What Is Trauma?
Trauma is more than a difficult memory, it is the mind and body’s emotional response to a profoundly distressing event, such as an accident, natural disaster, crime, or abuse. Initial reactions often include shock, denial, or disbelief, but trauma can also create long-lasting patterns of fear, avoidance, and disconnection if left unresolved.
Common Symptoms of Trauma
- Reliving the event through flashbacks or nightmares
- Flashbacks or intrusive memories
- Hyperarousal (always on edge, easily startled)
- Feeling emotionally numb or detached from others
- Avoiding people, places, or situations that bring reminders
- Being on edge, jumpy, or easily startled
- Struggling with trust and closeness in relationships
- Carrying heavy feelings of guilt, shame, or unworthiness
- Persistent anxiety, fear, or sadness that doesn’t seem to fade
Unlike bipolar disorder, trauma symptoms are often triggered by reminders of past experiences rather than cycling without context.
Read More: Intrusive Memories in PTSD: Causes, Triggers & Coping Strategies
Why Trauma Gets Mistaken for Bipolar
Dr. Reshie explains that trauma can mimic the up-and-down cycle of bipolar disorder:
“In trauma, you see people going up–becoming anxious, hyper, unable to sleep–and then crashing down into despair. On the outside, it looks like manic and depressive episodes, so doctors often label it as bipolar.” — Dr. Reshie Joseph
The danger is that once the bipolar label is applied, treatment usually becomes medication-heavy. This may suppress symptoms temporarily, but it does not address the underlying trauma.
Which Symptoms overlap between Trauma and Bipolar?
Because both conditions affect mood, energy, and thinking patterns, trauma and bipolar disorder can sometimes look alike. Recognizing these overlapping symptoms is important so people get the right support and treatment.
- Intense mood changes (emotional highs and lows)
- Irritability or anger outbursts
- Difficulty concentrating or staying focused
- Disturbed sleep (too little or too much)
- Low energy and fatigue
- Feelings of sadness, hopelessness, or guilt
- Risk-taking or impulsive behaviors
- Anxiety and restlessness
Read More: Reshie Joseph to Present New Trauma Recovery Model at NCPC 2025
Can Trauma cause bipolar?
Trauma itself doesn’t directly cause bipolar disorder, which is largely linked to genetics and brain function. However, traumatic experiences can worsen symptoms, trigger episodes, or make the diagnosis more complicated. In some cases, people with both trauma and bipolar disorder may need tailored treatment that addresses both conditions together.
The Cost of Misdiagnosis
When trauma is mistaken for bipolar disorder, the consequences can be severe. People may:
- Experience delays in receiving proper treatment, as their condition is misunderstood.
- Be prescribed inappropriate medications, such as antidepressants without mood stabilizers, which can trigger manic episodes.
- Continue struggling with trauma-related symptoms, like hyperarousal, irritability, poor concentration, and disturbed sleep, that medications alone cannot resolve.
- Face higher risks of harm, including suicidal thoughts or attempts, because the underlying trauma remains untreated.
- Suffer from worse overall functioning over time, as neither condition receives the right kind of care.
“By the time people come to me, they already know. They know the drugs aren’t working. They know something else is wrong. What I do is help them see it for what it really is–trauma.” – Dr. Reshie Joseph
Read More: Unlocking Trauma: Reshie Joseph’s Diathesis-Stress Model at NCPC Singapore 2025
Key Differences Between Trauma and Bipolar Disorder at a Glance
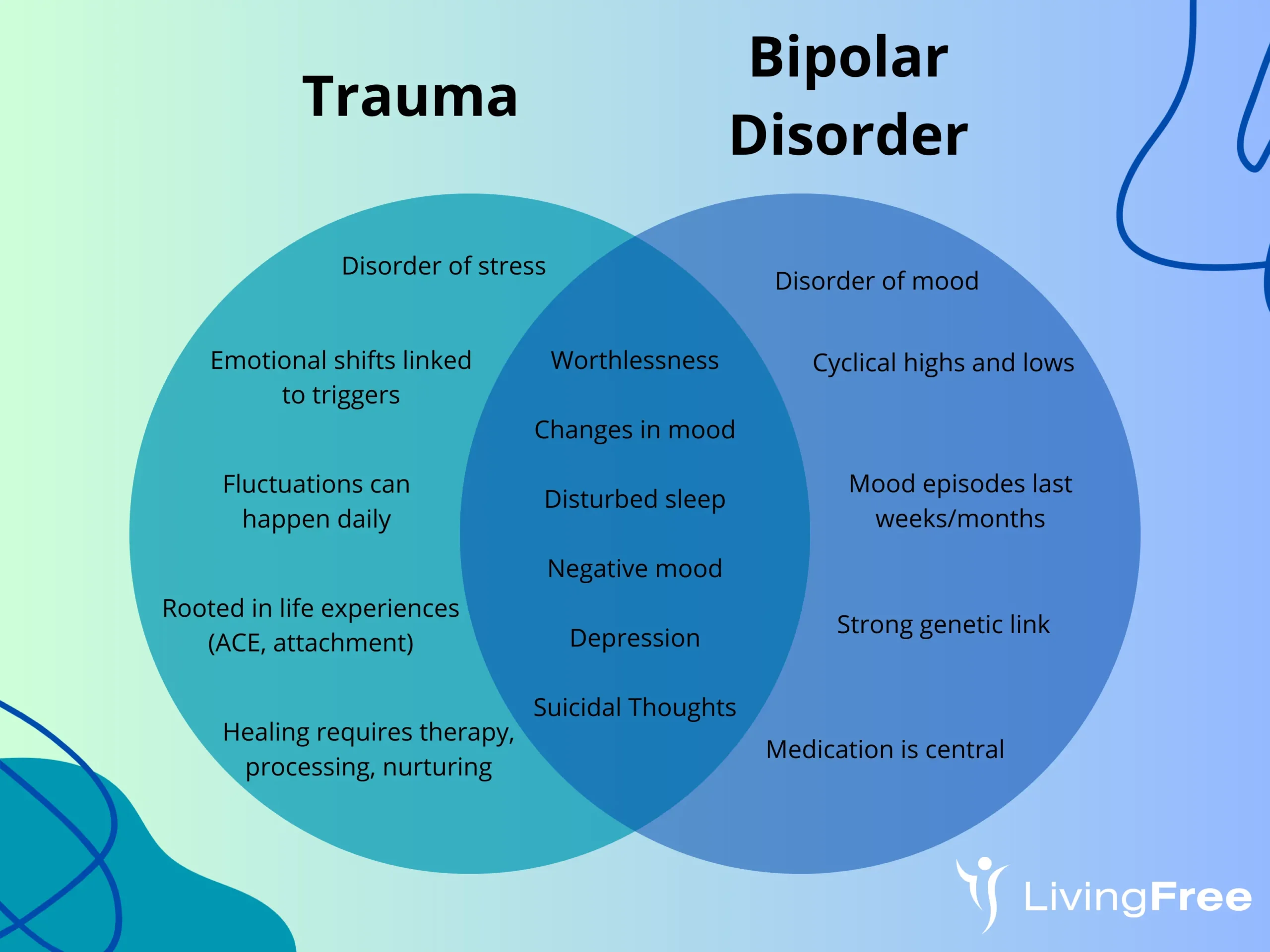
Although they are often mistaken or misdiagnosed, Trauma and Bipolar disorder are not the same. Above is a diagram of differences, and also the glances of overlaps.
A Way Forward
At Living Free, we believe the right diagnosis matters, but so does the right approach. Trauma can’t be medicated away. Healing requires:
- Safe and supportive relationships
- Working through memories at a pace the body can handle
- Building self-care and resilience practices
For many, simply naming trauma for what it is brings a powerful sense of relief.
“When I map trauma symptoms on the board, people say, ‘Doc, you’ve just written my life story.’ For the first time, they finally understand what’s wrong.” – Dr. Reshie Joseph
Conclusion
Trauma and bipolar disorder may look similar on the surface, but they are not the same condition. Misdiagnosis can keep people trapped in cycles of medication and despair. With the right understanding and care, it is possible to move beyond labels and begin a journey of genuine healing.
A qualified mental health provider can help with an accurate diagnosis and effective treatment options tailored to the needs. You don’t have to navigate this alone. You can contact us today if you or someone close to you is experiencing symptoms of trauma or bipolar disorder. Healing is possible, and every step forward is a step toward a brighter tomorrow!